“Mistakes are the growing pains of wisdom.”
— WILLIAM JORDAN
INTRODUCTION
The paramedic work environment is often high-pressure and fast-paced. This type of environment coupled with complex health conditions, emergency situations, and high-risk medication therapies can lead to significant errors in the appropriate administration of many medications (1). Patients, families, paramedics, and the healthcare system, in general, are highly affected by preventable medication errors (1).
Medication errors can lead to adverse drug events such as serious side effects, allergic reactions, overdose, and, in extreme cases, death (1). A study involving San Diego County paramedics showed that 9% of paramedics reported medication errors that occurred in the previous year (2). Out of the reported errors, 63% were dose-related errors, 33% were protocol errors, 21% were wrong route errors, and 4% were wrong medication errors (2). Additionally, 4% of these errors were not reported appropriately (2). It is important to be aware of potential medication errors, how they can happen in the prehospital environment, and steps that can be taken to avoid them.
CONTRIBUTING FACTORS FOR MEDICATION ERRORS
Taking every precaution possible to prevent medication error is always important, but certain scenarios tend to increase the chances of making an error.
The first includes patients who are receiving multiple medications (2). A patient receiving multiple medications is more complex than a patient receiving one, or no, medication (2). When dealing with a patient receiving more than one medication, it is important to check the name, dose, and administration route of the drug to avoid confusion and inappropriate administration (2).
The chance of a medication error is also increased when proper verification checks are skipped (2). It is often recommended to do a multi-step check of the medication, preferably with a second medic (2). A multi-step verification can take valuable time and can be forgotten or intentionally skipped (2). Proper verification checks are especially important when using medications that are unfamiliar or those that are infrequently used (2).
Dosage calculations are also a contributing factor to a medication error (2). When calculating a dose, perform the calculation more than once and, if possible, with another paramedic to verify the accuracy of the answer (2).

TYPES OF MEDICATION ERRORS
There are many ways in which inappropriate medication administration can occur. A variety of factors must be considered before giving medication to a patient in order to guarantee effectiveness and safety. The following includes different examples of medication errors and their potential effect on a patient.
- The patient is given an incorrect dose (3)
- Administering medication at an appropriate dose is vital for patient safety. Examples include a patient requiring 100mg of medication, but they are accidentally given 200mg.
- The medication is not indicated (3)
- This type of error involves giving medication to a patient when they do not need it. This can lead to adverse effects and can worsen the condition of the patient. An example includes giving an antiarrhythmic medication to a patient in cardiac arrest with pulseless electrical activity.
- The patient is given the wrong drug (3)
- When proper time is not taken to verify a medication, the patient can potentially be given the wrong medication. This puts the patient at risk for adverse events and their condition can worsen significantly if appropriate medications are not given quickly.
- The drug is not diluted/prepared appropriately (3)
- Some medications require dilution before administering to reach the appropriate dose of medication. If a medication is not diluted prior to administration, this can lead to overdose or significant adverse events.
- Failure to administer an appropriate drug (3)
- Protocols often describe the exact medications and steps that should be taken to appropriately care for a patient in an emergency setting. Failure to administer a protocol-prescribed medication puts the patient’s condition at high risk for worsening.
- The drug is administered via an inappropriate route (3)
- It is important to pay special attention to liquid drugs that are injectable. High levels of attention should be given to whether the medication should be given via intramuscular or intravenous routes, or if it should be injected at all.
- The medication is contraindicated (3)
- A contraindicated medication is prohibited in a patient. This may be due to the patient’s known allergies, pregnancy status, or other clinical factors related to their presentation.
- The medication is expired (3)
- Medication expiration dates should be checked prior to administration in order to be sure that a patient is not given an expired medication. Expired medications lose effectiveness and are not guaranteed to be safe for the patient.
- Incorrect timing (3)
- Medications often require repeat dosing to remain effective and treat the condition appropriately. Giving a repeat dose of medication too soon, or too late, can put the patient at risk for adverse events or can reduce the effectiveness of the medication.
- Pediatric dosage instructions are not followed (4)
- Studies have demonstrated an error rate of over 30% for medications administered to pediatric patients. Pediatric patients often have restrictions on the type of medications they can receive and the doses that are safe for this population. For example, a patient under 18 that is given an adult dose of a medication can lead to overdose and other serious adverse events.
A study observing Magen David Adom EMS service in Israel explored the type of errors that were seen most often in emergency vehicles (5). They found that most errors involved either administering a drug that was not indicated for the patient or giving an incorrect dose of the drug (5).

STRATEGIES TO HELP REDUCE FUTURE MEDICATION ERRORS
It is a fact that medication errors are preventable, unnecessary occurrences. Medication errors can be widely prevented by implementing strategies and safeguards to confirm that medication therapy is appropriate for each and every patient.
Five Rights
The first strategy is called “five rights”. The “five rights” are a technique often used by healthcare providers in order to make sure a medication is safely administered3. The “five rights” involves checking five different things (3):
- Right Patient – confirm that the patient receiving the medication is the correct patient.
- Right Drug – confirm the name of the drug that is being given to the patient.
- Right Dose – confirm that the dose is appropriate for the patient and that it is correct.
- Right Route – confirm that the route (oral, IM, IV) is appropriate for the patient and the drug.
- Right Time – confirm that the drug (or repeated dose) is given at the correct time.

THE TRIPLE CHECK/MEDICATION ADMINISTRATION CROSS CHECK
As mentioned above, a common strategy to confirm the appropriateness of a medication and administration technique is a triple check (2). The triple-check strategy has three steps:
- Check the medication, dose, and route that is planned to be given to a patient.
- Confirm this medication, dose, and route with the second medic.
- After the second medic confirms the appropriateness, perform a final check of the medication name, the dose, and how the medication should be administered for a total of three confirmations that this is correct (2).
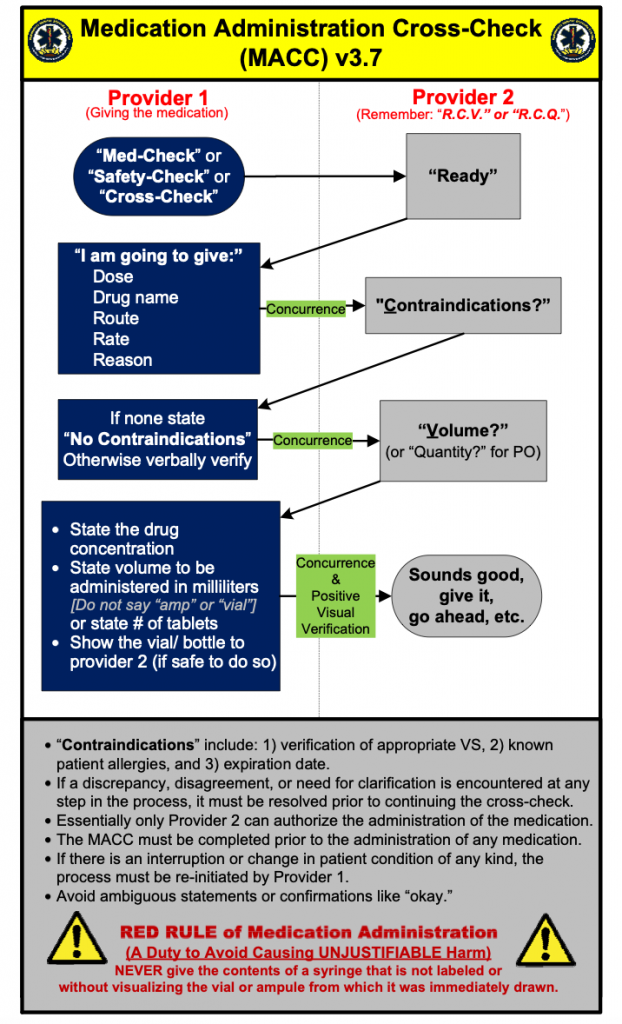
Similar to the triple check, a strategy called the Medication Administration Cross Check (MACC) was developed by Sedgwick County Emergency Medical Service (3). MACC is a standardized method of medication verification with the intention of reducing medication errors (3). MACC requires two providers to perform a medication or safety check. The steps of the safety check are as follows (3).
- Provider 1 lets Provider 2 know there is a safety check to be completed.
- Provider 2 then lets Provider 1 know they are ready.
- Provider 1 then lists the dose, drug name, route, rate (if applicable), and reason that the drug is being given.
- Provider 2 inquires about the presence of contraindications to the medication.
- Provider 1 confirms the absence of contraindications.
- Provider 2 requests a confirmation of the dose, volume, or quantity of medication being given.
- Provider 1 states the drug dose/concentration and volume to be administered in milliliters or the number of tablets.
- After visual verification of the vial/bottle, Provider 2 confirms that the medication is safe and can be given to the patient.
ADHERENCE TO PROTOCOLS
Many medication errors can be attributed to mistakes while following the protocol (2). This may be a wrong medication, misread dose, omission of appropriate medication, or other errors (2). Treatment protocols are in place to improve the efficacy and safety of treating specific conditions (2). Another benefit of protocols is that they reduce the pressure on the paramedic to confirm the correct therapy (2). Even when extremely familiar with protocols, it is important to ensure that every step is being followed to reduce the chances of making a medication error (2).
SPECIAL ATTENTION FOR PEDIATRIC DRUG DOSING
Pediatric drug dosing has a high rate of error in prehospital environments (4). In addition to the five-rights and triple-check strategies listed above, additional precautions can be taken to ensure pediatric medication safety (4,6). Safety precautions can be implemented such as pediatric drug cards with doses in milliliters, EMS specific references for pediatric safety, eliminating common pediatric drug calculations, and practicing weekly pediatric drug dosing problems (4,6).

DRUG CALCULATION SIMPLIFICATION AND DOUBLE-CHECK
Drug calculations continue to be a common source of medication error in the paramedic environment, especially when related to pediatric patients (2). Performing a second check on calculation or having a second medic confirm the accuracy of calculations can reduce potential medication error (2).
WELL LABELED DRUGS/DRUG STORAGE
Unorganized medications and medication labels may lead to errors (2). Organization and clearly labeled storage containers can help reduce common drug errors such as the wrong medication or the wrong dose given (2).
ERROR REPORTING
Even after appropriate precautions are taken and strategies are in place, errors will happen (2). It is important to report errors when they happen so the source of the error can be identified (2). Reporting errors can help identify the type of error that happened, the reason the error happened, and what areas can be improved to reduce the likelihood of the error happening in the future (2).
OTHER STEPS
In addition to these standard safety and quality verification steps that can be taken to reduce medication error, there are other steps that can be taken for extra assurance (1). If the patient is conscious and willing, the following steps may help improve patient safety and reduce errors (1).
- Inform the patient about drugs they are receiving
- Take a complete drug history
- Ask about medication allergies
- Consider any drug-drug interactions
- Document each drug administered
“Even after appropriate precautions are taken and strategies are in place, errors will happen.”
CONCLUSION
In summary, there is a high risk for medication errors among the paramedic environment. Taking the time to become educated about the different types of errors and implementing strategies to prevent them is vitally important for patient health and safety. Through consistent triple checking, calculation confirmations, error reporting, and more, medication errors can be dramatically reduced, and patient safety can be largely increased.
REFERENCES
- Crossman M. Technical and Environmental Impact on Medication Error in Paramedic Practice: A review of causes, consequences, and strategies for prevention. Australasian Journal of Paramedicine. 2009; 7(3): 1-10.
- Vilke GM, Tornabene SV, Stepanski B, et. al. Paramedic Self-Reported Medication Errors. Prehospital Emergency Care. 2006; 10(4): 457-462.
- Misasi P and Keebler JR. Medication safety in emergency medical services: approaching an evidence-based method of verification to reduce errors. Ther Adv Drug Saf. 2019; 10: 1-14.
- Hoyle JD, Crowe RP, Bentley MA, et. al. Pediatric Prehospital Medication Dosing Errors: A National Survey of Paramedics. Prehospital Emergency Care. 2017; 21(2): 185-191.
- Lifshitz AE, Goldstein LH, Sharist M, et. al. The American Journal of Emergency Medicine. 2012; 30: 726-731.
- Bernius M, Thibodeau B, Jones A, et. al. Prevention of Pediatric Drug Calculation Errors by Prehospital Care Providers. Prehospital Emergency Care. 2008; 12(4): 486-494.
Written by Hayden Gharibyar, PharmD for MedCognition
MedCognition created PerSim, the holographic patient simulator made to help the frontlines of healthcare save more lives. EMS EDUCATION/ TRAININGSEPTEMBER 10, 2020